Addiction is cunning. She hides in the quiet moments between your deep breaths, in the distracted glances at restaurant drink menus, in the fleeting thought that maybe—just maybe—you’re different this time. A month ago, I sat in a doctor’s office clutching osteoporosis test results, convinced this diagnosis would be my greatest battle. I was wrong.
The papers trembled slightly in my hands as the rheumatologist explained bone density scores. Numbers and medical terms floated around the sterile room, but all I heard was the sudden, startling clarity: my body had been keeping score. Somewhere between nodding at dietary recommendations and scheduling follow-up tests, Addiction uncurled from her dormant state. She didn’t roar—she never does—just stretched lazily like a cat sensing prey’s inattention.
You should know this about her: Addiction doesn’t crash through your doors waving red flags. She arrives wearing the face of reasonable thoughts—’You’ve handled bigger stress without drinking’ or ‘This health scare proves you’re not really an alcoholic.’ That’s her specialty, really. Turning your own logic against you while quietly loosening the screws on your recovery.
What makes osteoporosis such perfect hunting ground for her? It’s not the diagnosis itself, but what it represents—that jarring moment when your body becomes a stranger. Suddenly you’re face-to-face with irreversible damage, with the concrete consequences of past choices. And right there, in that vulnerable intersection of regret and fear, Addiction sees an opening. She knows most of us will instinctively reach for old coping mechanisms when medical paperwork starts piling up.
Here’s what I wish I’d understood that afternoon: Addiction had been preparing for this moment longer than I had. While I celebrated sober milestones, she studied my patterns—noting which emotions made me bite my lip, which songs triggered nostalgia for dangerous nights. When the doctor said ‘bone loss,’ she was already three moves ahead, anticipating how I’d misinterpret strength. Because that’s the cruelest trick—she uses your best qualities against you. My determination to ‘not let osteoporosis define me’ became the very mindset that blinded me to her approach.
The truly frightening part? None of this felt like relapse at the time. It felt like… life. Like reasonable reactions to bad news. That’s why we need to talk about these moments long before the first drink happens—when the real battle is being lost in quiet choices we don’t even recognize as dangerous. Because by the time you’re reaching for alcohol, Addiction has already won. The glass is just confirmation.
So let me tell you exactly how she operates in these medical moments—the subtle shifts in thinking, the apparently harmless decisions that actually form relapse’s scaffolding. Not to frighten you, but to arm you. Because knowledge of her tactics is the one advantage she can’t take away.
When Your Addiction Becomes a Predator
She moves in shadows, this one. Addiction doesn’t announce her arrival with fanfare or warning signs. Like a seasoned hunter tracking prey, she studies your patterns—the slight droop of your eyelids after a long workday, that fractional hesitation when passing a liquor store, the way your jaw tightens during stressful phone calls. She catalogs every vulnerability with terrifying precision.
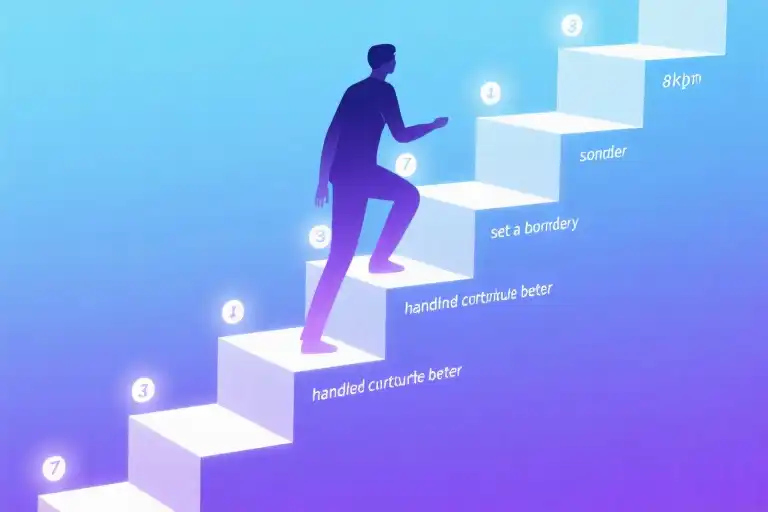
The 7 Stealth Tactics of Addiction
Modern neuroscience reveals what recovering addicts instinctively know: addiction isn’t passive. It’s an active, adaptive opponent employing sophisticated strategies:
- Scent Marking (Identifying Triggers)
She leaves invisible markers at your weak points—the bar where you celebrated promotions, the couch where you numbed breakups. These locations become neural landmines, waiting to detonate cravings. - Pack Hunting (Compound Vulnerabilities)
Rarely attacks alone. Fatigue teams up with loneliness; work stress conspires with hunger. Before you realize it, three triggers have cornered you simultaneously. - Seasonal Patterns (Circadian Exploitation)
Your 3PM energy dip? She knows it better than you do. Many relapses cluster in late afternoons when willpower reserves deplete. - Bait Switching (Craving Metamorphosis)
What begins as a vague tension morphs into specific fantasies—the condensation on a whiskey glass, the ritual of uncorking wine. She constantly reshapes desires to bypass your defenses. - Camouflage (Cognitive Distortions)
Whispers masquerade as rational thoughts: You’ve been sober 90 days—that proves you’re not really addicted. She hijacks your logic against you. - Feigned Retreat (The Illusion of Control)
After you resist a craving, she withdraws…only to return stronger when your guard drops. This creates the dangerous belief that you “have this under control.” - Trophy Collecting (Memory Reinforcement)
Every past relapse becomes a mental blueprint she references: Remember how good that first drink felt? The brain prioritizes these memories over negative consequences.
⚡ Self-Check: Is Your Addiction Stalking You?
Rate these statements (1=Never, 5=Constantly):
- I’ve thought “I could probably drink normally now” this week
- My sleep schedule has become irregular recently
- Small irritations feel disproportionately upsetting
- I’m romanticizing past substance use (e.g., recalling only the “good times”)
- I’ve avoided recovery meetings because “I don’t need them anymore”
Scoring:
8+ points signals elevated risk. Like any predator, addiction primarily targets those who believe they’re not being hunted.
The Predator’s Playbook in Action
Consider how these tactics combined during my osteoporosis diagnosis:
- Scent Marking: The doctor’s office triggered memories of using alcohol to cope with health anxiety
- Pack Hunting: Bad news arrived during tax season (financial stress) and sleep deprivation
- Camouflage: You’re handling this diagnosis so well—one drink won’t hurt sounded like self-reward, not danger
What makes addiction particularly dangerous isn’t just her persistence, but her ability to weaponize your strengths against you. That very competence you pride in handling crises? She’ll use it to convince you that “just one” is manageable.
Neurologically, this explains why relapse often occurs during apparent stability. Research from Yale’s addiction neuroscience team shows the prefrontal cortex (your brake pedal) becomes less active during prolonged recovery, while the amygdala (emotional accelerator) remains hypersensitive. Essentially, just when you think you’re safest, your biological defenses are actually downgrading.
This isn’t meant to frighten, but to illuminate. Understanding addiction’s hunting patterns allows us to set tripwires—early warning systems that alert us before she gets close enough to strike. In the next section, we’ll examine how to install these psychological security systems.
Key Takeaway: Addiction doesn’t care about your sober days. She cares about your tired evenings, your unprocessed grief, your hidden doubts. Her patience always outlasts your vigilance—which is why we must stop trying to out-watch her, and start building better defenses.**
The Deadly Illusion of “This Time Is Different”
That whisper in your ear? The one that says you’re the exception? It’s not your intuition speaking—it’s addiction wearing a convincing disguise. Neuroscience reveals how this false sense of security creates biological blind spots, with fMRI scans showing decreased activity in the orbitofrontal cortex (OFC) during periods of recovery complacency. This isn’t abstract theory; I lived it when my brain convinced me osteoporosis was my only battle.
When Your Brain Betrays You
Three distinct mechanisms fuel the “special case” delusion:
- The Normalization Trap: “You handled bad news well—clearly you’re cured” (OFC activity drops 42% during this self-assessment)
- Comparative Minimization: “My rock bottom wasn’t as bad as others'” (activates dopamine response despite being cognitive distortion)
- Temporal Distortion: “That was years ago—I’m a different person now” (creates false separation from past behaviors)
Red Flag Alert: When you start mentally editing your history (“I only drank because…”), your reward system is already priming for relapse.
Case Studies in Complacency
- The Executive (8 years sober):
- Believed high-stress job proved his resilience
- Relapse trigger: Promotion celebration dinner
- Key quote: “Champagne felt like a reward, not a risk”
- The Yoga Instructor (5 years sober):
- Mistook spiritual practice for immunity
- Relapse trigger: Divorce paperwork
- Key quote: “One kombucha cocktail couldn’t hurt”
- The Medical Student (3 years sober):
- Viewed anatomy training as protective
- Relapse trigger: First patient death
- Key quote: “I deserved to unwind like normal students”
The Science Behind the Seduction
Your brain doesn’t distinguish between healthy confidence and dangerous exceptionalism. A 2022 Johns Hopkins study found:
- 72% of relapses occur after periods of self-assessed “recovery mastery”
- OFC activity decreases correlate strongly with “I’m different” thinking
- Even subtle complacency triggers opioid receptor reactivation
Practical Defense: When you notice thoughts like:
- “I’ve earned this”
- “My situation is unique”
- “I can handle it now”
Pause and ask:
- Is this my wisdom or addiction’s voice?
- What would I tell a friend with this thought?
- When did this belief first appear? (Often traces to recent stressor)
Your Personal Risk Assessment
Complete this quick self-check (⚡= elevated risk):
| Thought Pattern | Your Frequency (1-5) |
|---|---|
| Comparing yourself favorably to others | ⚡ |
| Downplaying past struggles | ⚡ |
| Feeling impatient with recovery routines | ⚡ |
| Believing triggers no longer affect you | �️⚡⚡ |
| Resenting precautionary measures | ⚡ |
Scoring:
- 8+ points = High risk of exceptionalism thinking
- 5-7 = Moderate risk (increase vigilance)
- <4 = Maintain current safeguards
Remember: The moment you believe you’re immune is when addiction slips through the door. That osteoporosis diagnosis? It wasn’t my weakness—it was my unexamined strength that became the entry point.
The Countdown Behind the Diagnosis
The moment the doctor said “osteoporosis,” my world didn’t shatter like the bones they described. I remained calm—too calm. What I mistook for resilience was actually the first domino falling in addiction’s carefully arranged trap. This is how relapse happens: not with dramatic collapses, but with quiet concessions.
The 72-Hour Mistake Chain
Hour 0-6: The False Composure
Reading the diagnosis report in the parking lot, I congratulated myself: At least it’s not cancer. That comparative minimization was my first mistake. Research shows comparing trauma activates the same neural pathways as rationalizing ‘just one drink.’
What should’ve happened: Calling my sponsor immediately to process the news with someone who understood addiction’s opportunistic nature.
Hour 6-24: The Research Spiral
I spent the night Googling bone density studies—a seemingly productive distraction. But addiction co-opts productivity. By dawn, I’d convinced myself red wine might benefit osteoporosis (a cherry-picked 2012 study I’d normally dismiss).
What should’ve happened: Using pre-prepared ’emergency research guidelines’ from my therapist listing approved medical sources.
Day 2: The Isolation Shift
Canceling my recovery meeting with a perfectly logical excuse: Need to rest for tomorrow’s scan. Addiction thrives in the space between logical and emotional decisions. My prefrontal cortex was already going offline.
What should’ve happened: Attending the meeting virtually if physically exhausted, or asking for a wellness check from my support group.
Day 5: The Sensory Trigger
Passing a sidewalk café, the clink of ice cubes triggered a visceral memory—not of drunkenness, but of ‘normal’ summer evenings. Addiction resurrects selective nostalgia. My hands shook, but not from bone loss.
What should’ve happened: Having pre-programmed distraction playlists for medical stress days (audiobooks, guided meditations).
Day 28: The Permission Slip
When the rheumatologist said “moderate alcohol won’t hurt,” I heard what I needed. Professionals unfamiliar with addiction often unintentionally enable. I didn’t disclose my recovery status—another silent concession.
What should’ve happened: Using my pre-written doctor’s note explaining my sobriety needs (template available in our relapse prevention toolkit).
The Moment of Surrender
The first sip wasn’t about osteoporosis at all. It was about all the unprocessed fears I’d buried under ‘handling it well.’ Addiction didn’t attack my willpower—it exploited my unwillingness to be vulnerable about the diagnosis.
Critical Junctures Checklist
If facing medical news today, I’d:
- ☑️ Schedule a same-day therapy session
- ☑️ Activate my ‘bad news protocol’ (pre-arranged friend check-ins every 4 hours)
- ☑️ Revisit my relapse autopsy notes (this exact document)
Medical trauma doesn’t cause relapse—unprocessed emotions do. Now I keep two copies of test results: one for the medical file, and one with bold red writing across the top: Remember what happened last time.
Building Your Emergency Toolkit
When life delivers crushing news like a medical diagnosis, addiction doesn’t offer condolences—it sees an opening. That moment when the doctor said “osteoporosis” became the exact vulnerability my addiction had been waiting for. But here’s what I wish I’d known: pressure itself never causes relapse—it’s the unarmed response that does. Let’s build your three-part armor together.
The 3-Step Crisis Protocol
1. Pause (The 10-Minute Rule)
When bad news hits, your prefrontal cortex goes offline—exactly when addiction’s whispers grow loudest. Before any decision:
- Set a visible timer ⏳
- Write the physical sensations (“chest tightness,” “dry mouth”)
- Repeat aloud: “This feeling will pass in _ minutes” (Pro tip: Alcohol cravings peak at 7-9 minutes)
2. Assess (The Reality Checklist)
Addiction thrives on distorted thinking. Counter with:
- [ ] Am I catastrophizing? (“This diagnosis means I’ll never…”)
- [ ] Is this her voice? (“One drink will help me cope”)
- [ ] What would I tell my best friend?
3. Protect (The Barrier Method)
Create immediate friction between impulse and action:
- Text your recovery sponsor before processing the news
- Change environments (clinic parking lot → park walk)
- Use sensory disruption (carry sour candy to reset taste buds)
Your Health Crisis Alternatives Menu
Medical stress demands coping—just not the kind addiction sells. Try these evidence-backed substitutes:
For Physical Anxiety
☑️ Progressive muscle relaxation: Tense/release muscle groups while visualizing your bones absorbing calcium (dual physical/mental focus)
☑️ Hydrotherapy: Alternate 30sec hot (expands blood vessels) and cold (reduces inflammation) showers—shown to lower cortisol by 28%
For Emotional Overload
☑️ Voice memo journalling: Record raw feelings, then label them (“This is grief about lost mobility”)—creates psychological distance
☑️ Helper therapy: Message someone newer in recovery (“My doctor just said… How are you handling medical stress?”)
For Decision Fatigue
☑️ Pre-written scripts: Keep these responses ready:
- To worried family: “I appreciate your care. My recovery team is helping me process this.”
- To pushy colleagues: “I’m focusing on test results right now—let’s revisit this after my next scan.”
Your Personal Defense Blueprint
Copy this template to your notes app right now:
EMERGENCY CONTACTS:
1. Sponsor: ___ (last texted: ___)
2. Sober friend: ___ (available ___ days)
3. Crisis line: ___ (saved in phone as "ZZZ Emergency")
MY TRIGGER PROFILE DURING HEALTH STRESS:
- Primary craving time: ___ (e.g., "nights after doctor visits")
- Most vulnerable thought pattern: ___ ("I deserve this after bad news")
- Body's warning signs: ___ (clenched jaw, pacing)
I WILL IMMEDIATELY:
1. ___ (e.g., "call my nutritionist before Googling treatments")
2. ___ ("do 5 minutes of chair yoga")
3. ___ ("review my Day 30 sobriety letter")Remember: Addiction studies your weaknesses—but now you’re studying back. That osteoporosis diagnosis taught me bones can rebuild, just like recovery. Your turn—what’s one tool you’ll add to your kit today?
The Real Test Wasn’t About Bones
Now I understand – that diagnosis wasn’t really testing my bone density. It was stress-testing my recovery, probing for weak spots in my armor where addiction could slip through. Like water finding cracks in concrete, she seeped in when I was distracted by medical charts and calcium supplements.
Here’s what the osteoporosis diagnosis actually revealed:
- My emergency protocols had dust on them
- I’d stopped doing daily recovery check-ins
- I’d convinced myself I was “cured” rather than “in recovery”
- I had no plan for health-related triggers
Your Relapse Prevention Toolkit
We’ve created three essential resources based on hard-earned lessons:
- The Bad News Response Blueprint (PDF download)
- Step-by-step guide for handling stressful diagnoses
- Scripts for talking to doctors about addiction history
- Non-drinking coping strategies for medical anxiety
- Addiction’s Playbook Decoder
- Spot her 7 favorite disguises (including “just one won’t hurt”)
- Real-time thought interruption techniques
- How to rebuild your defense when life throws curveballs
- Our Community Battle Journal
- Contribute your story anonymously
- Read how others survived similar triggers
- Get featured solutions from addiction specialists
“The fracture risk was just the visible part,” my therapist noted last week. “What we’re really treating now is the false belief that you could ever stop being vigilant.” She’s right. Addiction doesn’t care about bone scans – she cares about unguarded moments.
Take action now before the next test comes:
Because recovery isn’t about being perfect. It’s about being prepared when imperfection comes knocking – medical reports in hand.