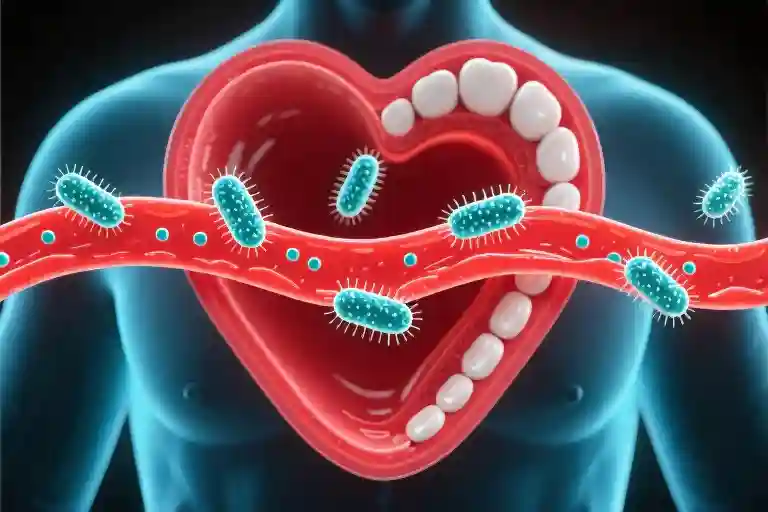
The human heart, no larger than your clenched fist, performs a silent miracle over 100,000 times each day. This relentless rhythm powers every moment of our lives, yet its precision makes it vulnerable – especially when microscopic invaders from an unexpected source come knocking. Recent research from Hiroshima University reveals something startling: the same bacteria we brush away each morning can travel through our bloodstream and settle in cardiac tissue, directly contributing to atrial fibrillation (AFib), that dangerous irregular heartbeat affecting millions.
What makes this discovery particularly unsettling is how ordinary the entry point appears. Those occasional traces of pink in the sink after flossing? Potential gateways for oral bacteria to begin their covert journey toward the heart. The study tracked this migration path with scientific precision, showing how periodontal pathogens bypass the body’s defenses, triggering inflammatory responses that disrupt the heart’s electrical signaling system.
We’ve long understood the cardiovascular risks of poor diet or sedentary lifestyles, but the toothbrush connection feels different – more intimate, more immediate. Nearly 60 million people worldwide now live with AFib’s consequences, a number that’s nearly doubled in just nine years even as global population grew only 10%. In the U.S. alone, 10.5 million adults (about 1 in 20) navigate the increased risks of stroke, heart failure, and dementia that accompany this condition.
Yet here’s the hopeful counterpoint: unlike genetic predispositions or environmental factors we can’t control, oral hygiene sits firmly in our daily routine. The Hiroshima findings suggest those two minutes morning and night might represent more than fresh breath – they could be safeguarding the steady rhythm that keeps us alive. As you reach for your toothbrush tonight, consider this: that simple bristle-and-paste ritual may be the most important cardiac care you’ll perform all day.
The Silent Journey: How Oral Bacteria Reaches Your Heart
Gum tissue isn’t just pink decoration in your mouth – it’s a carefully guarded border crossing. When that border becomes compromised through bleeding gums or microscopic tears from aggressive brushing, something remarkable happens. Bacteria that normally live harmlessly in your mouth suddenly gain access to a highway system they were never meant to travel: your bloodstream.
Researchers at Hiroshima University made this invisible journey visible through an elegant experiment. They tagged common oral bacteria with fluorescent markers and observed their path in animal models. Within hours, these glowing microbes appeared in the heart tissue, particularly clustering around the delicate electrical nodes that maintain our heartbeat’s rhythm. It’s as if these bacterial travelers had GPS coordinates pre-programmed for cardiac tissue.
What happens next reads like biological sabotage. The immune system detects these bacterial interlopers and launches an inflammatory response. This inflammation creates microscopic scars in the heart’s conduction system, like static on a phone line. The heart’s carefully choreographed electrical impulses begin misfiring, resulting in the erratic quivering of atrial fibrillation rather than strong, coordinated beats.
Three key mechanisms make this possible:
- Bacterial Adhesion: Certain oral bacteria like Porphyromonas gingivalis have surface proteins that act like molecular Velcro, allowing them to stick to heart tissue.
- Inflammatory Cascade: The body’s defense mechanisms ironically cause collateral damage, releasing enzymes that degrade cardiac tissue.
- Electrical Disruption: Scar tissue formation physically blocks the smooth transmission of electrical impulses across heart muscle.
This isn’t theoretical – cardiac surgeons routinely report finding oral bacteria species in the plaque removed from heart valves during operations. The path from bleeding gums to irregular heartbeat isn’t just possible; it’s been documented in peer-reviewed studies across multiple countries. What we once considered separate systems – mouth and heart – are in constant conversation through this bacterial exchange.
The frightening efficiency of this process explains why dentists notice something peculiar: patients with periodontal disease often show early signs of heart rhythm disturbances before their primary care physicians detect any cardiac issues. Your mouth might be sounding alarms your cardiologist can’t yet hear.
The Domino Effect of Atrial Fibrillation
The human heart operates with such remarkable precision that we rarely notice its rhythm—until something goes wrong. Atrial fibrillation isn’t just an irregular heartbeat; it’s a cascade of health consequences that can permanently alter lives. That five-fold increase in stroke risk we casually cite? It translates to real people like Michael, a 58-year-old architect who suddenly lost the ability to speak mid-presentation when a blood clot formed in his fibrillating heart and traveled to his brain.
What makes AFib particularly insidious is how it compounds damage across multiple systems. The chaotic quivering of the heart’s upper chambers allows blood to pool and clot. When those clots break free, they don’t discriminate—they might lodge in cerebral arteries causing strokes, or travel to kidneys contributing to chronic renal disease. The heart itself becomes less efficient over time, working harder while delivering less oxygen, which explains why AFib patients face double the risk of heart failure compared to those with normal rhythms.
Beyond the physical toll, the financial impact reverberates through households and healthcare systems. Annual treatment costs in the U.S. exceed $6 billion, with hospitalizations accounting for nearly 70% of expenditures. A single AFib-related stroke can cost $140,000 in acute care and rehabilitation—enough to pay for a lifetime of premium electric toothbrushes and dental checkups. Yet most insurance plans still classify periodontal treatment as cosmetic rather than preventive care, creating perverse financial disincentives for comprehensive oral health.
The cognitive connection often gets overlooked. Research shows AFib patients have a 30% higher likelihood of developing dementia, likely due to repeated micro-strokes that chip away at brain function over time. Imagine losing not just physical independence but cherished memories—family vacations, grandchildren’s birthdays, the melody of your wedding song—because oral bacteria triggered a chain reaction no one thought to prevent.
What stays with me aren’t just the statistics but the human stories behind them. Like Sarah, who survived her stroke but can no longer play piano duets with her daughter. Or James, whose AFib-induced kidney damage means spending twelve hours weekly hooked to a dialysis machine instead of fishing with his grandsons. These aren’t hypothetical risks—they’re stolen moments that proper flossing might have preserved.
Perhaps most frustrating is how late many discover the connection. By the time someone receives an AFib diagnosis, the oral bacteria that may have contributed have already done their damage. This isn’t about fear-mongering—it’s about recognizing that the two minutes we spend brushing morning and night might be the most important health investment we never knew we were making.
The Silent Surge: Mapping AFib’s Global Footprint
The numbers tell a story we can’t afford to ignore. Between 2010 and 2019, while the world’s population grew by a modest 10%, cases of atrial fibrillation nearly doubled – from 34 million to 60 million globally. This isn’t just statistical noise; it’s a silent epidemic rewriting cardiovascular health narratives across continents.
The Geography of Risk
Regional patterns emerge when we plot AFib prevalence:
- North America accounts for nearly 20% of global cases, with approximately 10.5 million American adults (5% of the population) living with the condition
- Europe shows particularly high rates in aging populations like Germany and the UK
- Asia presents a curious dichotomy – while China’s cases rise with Westernized lifestyles, Japan maintains surprisingly low rates (more on that later)
What makes these patterns particularly concerning is how they track with another invisible health crisis: periodontal disease. The overlap isn’t coincidental. Researchers now see oral inflammation as one of the modifiable risk factors in this complex equation.
The High-Risk Profile
Three factors create a perfect storm for AFib development:
- Age: Risk increases sharply after 65, with about 9% of octogenarians affected
- Periodontal disease: Chronic gum inflammation doubles AFib risk according to Hiroshima University’s longitudinal studies
- Diabetes: This metabolic condition compounds risk by accelerating vascular damage
The synergy between these factors explains why AFib has become the arrhythmia equivalent of a slow-motion pandemic. When oral bacteria enter the bloodstream (a common occurrence in gum disease), they don’t just affect the heart in isolation – they amplify existing vulnerabilities.
The Japanese Exception
Japan’s relatively low AFib rates (about 30% lower than Western counterparts) offer intriguing clues. Two cultural habits stand out:
- Routine dental visits: 70% of Japanese adults see dentists preventively versus 40% in the U.S.
- Traditional diets: Omega-3 rich seafood may counteract inflammatory processes
This isn’t to suggest mouthwash can replace cardiology medications. But it does reinforce what preventive cardiologists increasingly emphasize: heart health begins with habits we often overlook. Your toothbrush might be the most affordable cardiovascular tool you own.
The global AFib surge mirrors another troubling trend – the rise of inflammatory diseases across industrialized nations. As we’ve outsourced food preparation and deprioritized preventive care, our bodies pay the price in unexpected ways. The connection between oral bacteria and cardiac rhythm disorders serves as a reminder: human health operates as an interconnected system, not a collection of isolated parts.
What makes these statistics particularly urgent is their trajectory. At current growth rates, AFib could affect 12 million Americans by 2030. The economic burden already exceeds $60 billion annually in treatment costs and lost productivity. Yet much of this may be preventable through interventions as simple as proper flossing technique and regular dental cleanings.
In our next section, we’ll translate these insights into practical defense strategies – because understanding risk matters less than taking action against it.
Your Oral Defense Playbook
The connection between oral hygiene and heart health isn’t just theoretical—it’s actionable. Here’s how to transform your daily routine into a shield against systemic inflammation and cardiac risks.
The 6-Angle Brushing Method
Most people brush with random scrubbing motions, missing nearly 40% of tooth surfaces. Try this dentist-approved approach:
- 45-degree gumline angle: Tilt bristles toward gums to disrupt plaque biofilm
- Short back-and-forth strokes: Cover no more than 2 teeth at a time
- Inner surfaces first: These often get neglected when energy wanes
- Chewing surfaces: Use firm circular motions to clean pits and fissures
- Tongue sweep: Gently brush from back to front to remove bacteria
- Two-minute minimum: Divide your mouth into quadrants (30 seconds each)
Electric toothbrushes with pressure sensors can automate angle maintenance, with clinical models like Oral-B iO ($200-$300) showing 100% better plaque removal than manual brushing in studies.
Flossing: The Silent Guardian
That innocent-looking dental floss does more than dislodge food particles—it disrupts bacterial colonies before they enter your bloodstream. Common mistakes to avoid:
- Skipping back molars: These teeth account for 60% of chewing surfaces yet receive the least attention
- Sawing motions: This traumatizes gums; instead use C-shaped wrapping around each tooth
- Rinsing after flossing: You’re washing away dislodged bacteria—just spit instead
For those who struggle with traditional floss, water flossers like Waterpik ($50-$100) reduce gingivitis by 50% more than string floss alone according to Journal of Clinical Dentistry.
The Dentist-Approved Toolkit
Beyond basics, these tools create multi-layered defense:
- Antimicrobial mouthwash (e.g., Listerine Ultraclean, $8): Reduces oral bacteria by 99% for 12 hours
- Tongue scrapers ($5-$15): Remove 75% more volatile sulfur compounds than brushing alone
- Interdental brushes ($10/pack): Essential for gum recession areas where floss can’t reach
- Chewing gum with xylitol ($5/pack): Stimulates saliva flow that neutralizes acids
A surprising hero? Your kitchen timer. Setting it for 2 minutes increases brushing effectiveness by 26% compared to unmeasured brushing (American Dental Association data).
Maintenance Rhythm
Think of oral care like changing your car’s oil—regularity matters more than heroic occasional efforts:
- Every 6 months: Professional cleaning to remove tartar even perfect brushing misses
- Every 3 months: Replace toothbrush/electric brush heads (sooner if bristles splay)
- Weekly: Check gums for bleeding—the earliest warning sign of trouble
This isn’t about achieving Instagram-perfect teeth. It’s about recognizing that the same bacteria causing morning breath could be taking the express lane to your heart. Tonight when you brush, imagine each stroke sweeping away not just food particles, but potential heart rhythm disruptors. Your cardiovascular system will thank you with every steady, uncomplicated beat.
Your Oral Health Action Plan
Gum bleeding with morning breath isn’t just unpleasant—it’s your body waving red flags. Those minor irritations might be the first whispers of a conversation between your mouth and heart you’d rather not hear. The good news? You hold the power to change this dialogue.
Start tonight. Those extra two minutes with your toothbrush aren’t about achieving dentist-approved aesthetics—they’re a tangible investment in your cardiac future. Think of it as depositing coins in a health savings account where compound interest pays out in steady heartbeats. The mechanics are simple: angle your brush at 45 degrees to the gums, use gentle circular motions, and don’t rush the process like you’re scrubbing burnt toast. Your molars deserve the same attention as your front teeth, even if they don’t appear in selfies.
Flossing often gets treated like dental homework—something we pretend we’ve done when questioned. Here’s the shift: view it as preventative maintenance, like changing your car’s oil before the engine seizes. The C-shaped glide technique matters more than frequency—properly hugging each tooth surface removes what brushing misses. If traditional floss feels fiddly, water flossers with pulsating streams offer an effective alternative, particularly for those with braces or dental work.
Your toolkit matters. Fluoride toothpaste isn’t a marketing gimmick—it actively remineralizes enamel and disrupts bacterial growth. Electric toothbrushes with pressure sensors prevent gum damage while ensuring thorough cleaning. Don’t overlook tongue scrapers; that white coating harbors bacteria contributing to both bad breath and systemic inflammation.
Mark your calendar for professional cleanings like you would important meetings. Even meticulous home care can’t remove all tartar buildup, and those biannual visits allow early detection of gum disease—the stealthy gateway for oral bacteria entering your bloodstream. If budget allows, consider periodontal charting at your next visit; it measures gum pocket depths like a dipstick checking your engine’s health.
Tonight’s simple ritual—those two minutes of brushing, that thirty seconds of flossing—carries weight beyond fresh breath. Each proper stroke disrupts the invisible migration of bacteria toward your heart. Consistency compounds; the skipped sessions you consider insignificant accumulate like unchecked credit card interest. Your heart, that relentless muscle contracting 100,000 times daily without prompting, relies on these mundane acts of prevention.
Quick Self-Assessment:
- Do gums bleed when brushing? (Even occasionally counts)
- Morning breath persists after brushing?
- Family history of heart disease or AFib?
Two ‘yes’ answers mean your oral care needs immediate upgrading.
For visual learners, the American Dental Association’s tutorial videos demonstrate proper techniques. Your future self—the one enjoying steady heart rhythms and uncomplicated health screenings—will thank present-you for these small, consistent acts of prevention.