I stood out in nursing school for all the wrong reasons, or perhaps the right ones, depending on who you ask. At nearly thirty, I was a decade older than most of my classmates, those bright-eyed teenagers who still carried the optimism of high school hallways into our lecture rooms. They spoke of calling and purpose, of childhood dreams to heal and comfort. I spoke of student loans and recession-proof employment, of practical needs over spiritual callings.
This wasn’t some divine mission for me—it was simple mathematics. The numbers added up to stability: a guaranteed job, a reliable paycheck, benefits that would cover my family. When I looked at the nursing curriculum, I didn’t see a higher purpose; I saw a practical solution to financial problems. The romanticized image of the Angel of Mercy never factored into my decision matrix. I wasn’t there to save humanity—I was there to pay my mortgage.
That distinction became my greatest professional asset. While others struggled with the emotional weight of our chosen field, I maintained the boundaries I’d built over a lifetime. I watched classmates and later colleagues crash under the weight of suffering they tried to shoulder personally. They didn’t just care for patients; they absorbed their pain, their fears, their frustrations with a broken system. The nursing profession consumes such souls without mercy, chewing up and spitting out those who mistake empathy for effectiveness.
The American Hospital Association reports that 62% of nurses experience burnout, and that was before the pandemic reshaped our understanding of healthcare exhaustion. The number undoubtedly climbs higher each year, making burnout less an occupational hazard and more an inevitable outcome. We enter this field knowing it’s not a matter of if we’ll break, but when.
What they don’t teach you in nursing school is how to build the emotional scaffolding necessary to survive. They teach clinical skills, medical terminology, patient care protocols—but they skip the chapter on preserving your humanity while surrounded by suffering. They forget to mention that you’ll need to become a different person when you pull on those scrubs, that the self who walks into the hospital must be separate from the self who goes home to family.
This career demands more than medical knowledge; it requires emotional fortification. The system expects nurses to be heroes while providing minimal support for the psychological toll. Management wants unwavering dedication despite inadequate staffing. Patients need compassion from caregivers who are given little space for their own emotional needs. And through it all, we’re supposed to maintain that brave face, that professional demeanor that says everything is under control even when the world is burning around us.
They never tell you that nursing isn’t just a job—it’s an identity you put on and take off like uniform layers. They don’t explain that some days, the weight of that identity will feel heavier than any patient you’ll ever lift. But they also don’t mention the strange satisfaction that comes from doing difficult work well, from finding strength you never knew you possessed, from building boundaries that protect not just yourself but your ability to care for others effectively.
This is the reality they leave out of the brochures and orientation packets: nursing will break you, but it will also build you into someone stronger than you imagined. The question isn’t whether you’ll survive—it’s what kind of survivor you’ll choose to become.
The Gap Between Classroom and Reality
Nursing school prepares you for many things—anatomy charts, medication calculations, sterile techniques. What it doesn’t prepare you for is the moment you realize your education bore little resemblance to the actual profession. We learned about ideal scenarios with compliant patients and adequate staffing. Reality offered something entirely different: complex human beings in various states of crisis, and systems that often seemed designed to hinder rather than help.
They never told us about the emotional toll of watching someone’s deterioration despite your best efforts. They never mentioned how it feels to hold a stranger’s hand during their final moments because their family couldn’t arrive in time. They certainly never explained that you’d need to develop a separate professional persona—someone who could witness tremendous suffering without breaking, who could make life-altering decisions under pressure, who could compartmentalize so effectively that the woman who walked into the hospital barely resembled the one who walked out.
The most significant omission was the cost. Not the financial investment in education, but the personal expenditure required to sustain this career. They never told us that 62% of nurses experience burnout according to American Hospital Association data collected before the pandemic—a number that has undoubtedly climbed higher in recent years. They never explained that burnout isn’t an individual failing but an occupational hazard, something that waits for nearly everyone in this field regardless of their dedication or skill.
They never mentioned the family sacrifices either—the soccer games missed because of mandatory overtime, the birthday dinners spent apart, the Christmas mornings where you’re wrapping gifts before your night shift instead of watching children unwrap them. They never told us that our children would learn to understand our absence better than we understood it ourselves, that they’d develop a maturity about our career demands that no child should need to possess.
What they did teach us was to advocate for our patients above all else—before our own needs, before our families’ needs, before our loyalty to the facility. While noble in theory, this instruction failed to account for the unsustainable nature of such sacrifice. It created a generation of nurses who believed putting themselves last was not just expected but required, who internalized the message that needing breaks, support, or boundaries indicated some fundamental lack of dedication.
The reality I encountered differed dramatically from the classroom narratives. Instead of feeling like a heroic caregiver making dramatic differences in patients’ lives, I often felt like a cog in a malfunctioning machine—jumping between tasks, documenting endlessly, and navigating bureaucratic obstacles that seemed designed to prevent actual caregiving. The system wanted warm bodies with licenses, not necessarily thinking, feeling professionals with insights about how to improve things.
This gap between expectation and reality creates a particular type of professional whiplash. You enter believing you’ll be performing meaningful work that makes a visible difference. You quickly learn that much of nursing involves fighting systems, managing unrealistic expectations, and dealing with the fallout of healthcare’s business priorities. The emotional reward of helping someone exists, but it’s often buried beneath administrative burdens and systemic challenges.
Understanding this disconnect early might have changed how I approached my career. It certainly would have helped me develop better coping mechanisms and set more realistic expectations. Instead, like most nurses, I learned through experience—through those moments of crashing disappointment when reality failed to match what I’d been taught to expect.
The truth about nursing isn’t that it’s not rewarding—it can be profoundly meaningful work. The truth is that the rewards come with costs that aren’t adequately discussed during education. Recognizing this gap between the idealized version of nursing and its reality is the first step toward building a sustainable career in healthcare—one that serves both patients and the professionals who care for them.
The Angel of Mercy Myth
The nursing profession has long been romanticized through the lens of the “Angel of Mercy” archetype—that selfless, ever-compassionate caregiver who exists solely to alleviate suffering. This idealized image permeates nursing school orientations, hospital marketing materials, and public perception. What they don’t tell you is how dangerously unsustainable this mythology proves in actual practice.
I watched countless colleagues—genuinely compassionate individuals who entered nursing with beautiful intentions—become casualties of this unrealistic expectation. The system, hospital administration, and patients themselves often unconsciously demand that nurses perform this angelic role, regardless of the physical, emotional, or psychological cost.
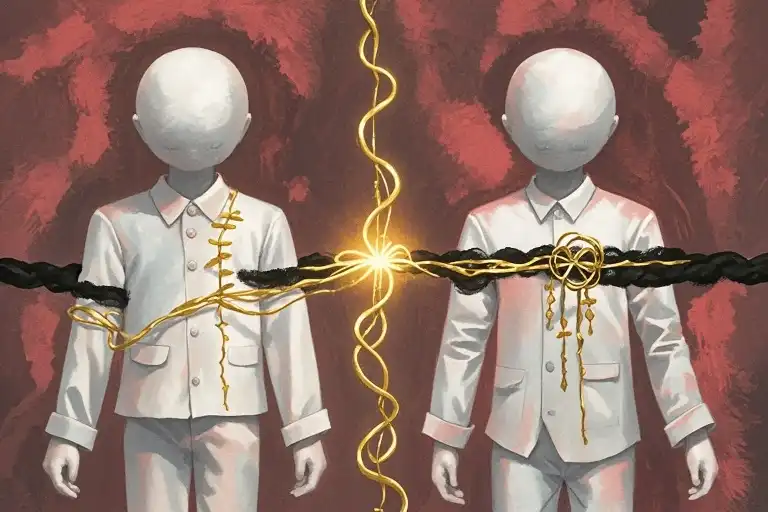
There’s a crucial distinction between empathy and compassion that nursing education often glosses over. Empathy—feeling what others feel—can become professionally hazardous when constantly exposed to trauma, grief, and suffering. Compassion—the desire to alleviate suffering while maintaining emotional boundaries—proves far more sustainable. The former drains you; the latter sustains you.
I recall a particularly gifted nurse named Sarah who embodied the Angel of Mercy ideal. She remembered every patient’s birthday, stayed late to hold hands with dying patients who had no family, and literally cried with families receiving bad news. Within three years, she left nursing entirely, emotionally bankrupt and diagnosed with severe depression. The system had consumed her compassion and offered nothing in return.
Another colleague, Mark, became so invested in his pediatric oncology patients that he began experiencing symptoms of the very cancers he was treating—a psychological phenomenon known as somatic symptom disorder. He’d show up in the emergency room convinced he had leukemia, only to be told it was stress-induced hypochondria. He eventually transferred to medical records, unable to continue direct patient care.
These weren’t weak individuals; they were some of the most caring professionals I’ve ever worked with. The tragedy wasn’t their capacity for connection but the system’s failure to protect that capacity. Nursing culture often subtly reinforces the message that setting boundaries means you care less, when in reality, boundaries are what allow you to care longer.
The American healthcare system operates on an unspoken agreement: nurses will absorb the emotional overflow that doctors don’t have time for, that hospitals don’t budget for, and that families can’t handle. We become the shock absorbers for the entire medical apparatus, and nobody checks whether those absorbers are worn out until they fail completely.
This mythology affects male nurses differently but equally profoundly. While female nurses face pressure to be nurturing angels, male nurses often confront expectations to be heroic protectors—strong, unemotional fixers who can handle any crisis without showing strain. Neither stereotype serves the actual humans behind the scrubs.
What makes the Angel of Mercy myth particularly insidious is how it frames self-care as selfishness. Taking mental health days, seeking therapy, or setting emotional boundaries gets interpreted as lacking dedication rather than demonstrating professional sustainability. I’ve watched charge nurses roll their eyes at colleagues requesting stress leave while praising those who worked through panic attacks.
The reality is that the most effective nurses I’ve known weren’t those who gave everything to every patient but those who learned to distribute their emotional resources strategically. They understood that compassion without boundaries is like a river without banks—it eventually floods everything and helps nobody.
This isn’t to suggest that nurses shouldn’t care deeply about their patients. The connection between caregiver and patient can be profoundly meaningful for both. But sustainable caring requires recognizing that you’re there to provide professional nursing care, not to become emotionally responsible for outcomes beyond your control.
The financialization of healthcare exacerbates this problem. As hospitals focus on patient satisfaction scores and press ganey ratings, nurses feel increased pressure to perform emotional labor that goes far beyond medical care. We’re expected to be therapists, family mediators, and spiritual guides—all while managing complex medical interventions and documentation requirements.
I learned early that my ability to remain in nursing depended on rejecting the Angel of Mercy mythology. I provided excellent clinical care, advocated fiercely for my patients, and treated everyone with dignity. But I didn’t take their pain home with me. I didn’t blame myself for outcomes I couldn’t control. I didn’t measure my worth by how emotionally drained I felt at shift’s end.
This approach wasn’t always appreciated. Some supervisors questioned my commitment when I declined extra shifts to preserve my mental health. Some families found me cold when I maintained professional boundaries during emotional moments. But thirty years later, I’m still here, while many of the “angels” have burned out completely.
The conversation needs to shift from expecting nurses to be self-sacrificing angels to supporting them as skilled professionals who deserve the same compassion they extend to others. This means adequate mental health resources, realistic patient ratios, administrative support for boundary-setting, and cultural change that values sustainability over martyrdom.
Nursing is already emotionally demanding enough without the added burden of mythological expectations. We need to replace the Angel of Mercy with a more realistic ideal—the competent, compassionate professional who knows that caring for others requires first protecting their own capacity to care.
The Art of Professional Boundaries in Nursing
Surviving twenty-six years in a Level 1 Trauma Center taught me more about self-preservation than any nursing textbook ever could. The emergency department doesn’t care about your feelings—it demands competence, resilience, and the ability to function amid chaos. What kept me standing when others fell wasn’t some innate heroic quality, but rather a carefully cultivated set of boundaries that became my professional armor.
I learned early that emotional investment in patients, while noble in theory, often leads to professional paralysis. The colleagues who crashed hardest were those who believed they needed to feel their patients’ pain to provide quality care. They’d take home the grief of failed resuscitations, the anguish of terminal diagnoses, and the frustration of systemic failures. Within months, some transferred to less intense units; others left nursing altogether.
My approach was different. I viewed emotional distance not as coldness but as professional necessity. When caring for a trauma patient, I focused on tasks: establishing IV access, monitoring vitals, administering medications. I allowed myself to care deeply about providing excellent clinical care without absorbing the emotional weight of each tragedy. This distinction—between caring for someone and carrying their pain—became my most valuable survival skill.
Department rotation emerged as my strategic defense against burnout. Every three to five years, when the emotional residue began accumulating, I’d transfer to a new specialty. From emergency to ICU, from surgery to recovery—each move provided a psychological reset. The change in patient population, workflow dynamics, and clinical challenges offered renewal without leaving the profession I’d come to respect.
This rotational strategy served multiple purposes. It prevented the complacency that sometimes accompanies mastery, continually pushing me to learn new skills. It exposed me to different management styles and hospital cultures, helping me identify toxic environments before they could damage my mental health. Most importantly, it allowed me to reinvent my professional identity periodically, shedding the accumulated stress of previous assignments.
Boundary-setting extended beyond patient interactions to include management expectations. I learned to say no to extra shifts when I felt depleted, despite the guilt trips about “abandoning the team.” I stopped checking work emails on days off and became disciplined about using my vacation time. These might sound like small rebellions, but in a culture that glorifies self-sacrifice, they were radical acts of self-preservation.
The physical boundaries mattered too. I developed rituals to mark the transition between work and home. Changing out of scrubs before leaving the hospital, taking a longer route home to decompress, sometimes sitting in the driveway for five minutes just breathing—these small practices created psychological space between professional demands and personal life.
What nursing school never taught us is that boundaries aren’t walls that isolate us from patients; they’re filters that allow us to give compassion without being destroyed by it. I could genuinely comfort a grieving family member while maintaining the emotional stability needed to care for my next patient. I could advocate fiercely for a patient’s needs without internalizing the frustration when the system failed them.
This boundary art isn’t about becoming numb—it’s about becoming sustainable. The healthcare system will always demand more: more hours, more emotional labor, more flexibility. Without clear boundaries, nurses become empty vessels, pouring from cups that never get refilled. I watched too many compassionate caregivers become bitter, exhausted shadows of themselves because they never learned to protect their own humanity while caring for others.
My rotation strategy wasn’t without professional costs. I sacrificed the deep expertise that comes with decades in one specialty and occasionally faced skepticism from colleagues who viewed my moves as lack of commitment. But the trade-off—mental health and career longevity—proved infinitely valuable.
Twenty-six years later, I understand that my boundaries weren’t limitations on my compassion but rather the framework that allowed it to endure. They enabled me to witness profound human suffering without being destroyed by it, to provide competent care without romanticizing the profession, and to eventually retire with both my pension and my psyche intact.
The unspeakable truth of nursing is that the system will break you if you let it. Boundaries aren’t selfish—they’re the necessary infrastructure for a sustainable career in healthcare. They’re what allow us to keep showing up, shift after shift, without losing ourselves in the process.
The System’s Relentless Demands
Hospital administration operates on a simple, brutal calculus: warm bodies equal staffing. In the operating room where I spent many years, we had a darkly humorous saying about calling in sick. You couldn’t just call out dead—you had to specify “cold and dead” because if you were still warm, they’d find someplace to put you to work. This wasn’t mere gallows humor; it was our reality, a reflection of how healthcare institutions view their nursing staff.
The staffing crisis in nursing isn’t occasional—it’s perpetual. Department managers spend their shifts playing musical chairs with personnel, constantly trying to cover gaps with insufficient resources. What this means for nurses is that our lives become permanently tethered to the facility’s staffing needs. That carefully planned family vacation? It might disappear if someone else calls in sick. Those promised days off? Suddenly revoked because the unit is short-staffed. We learned to view our phones with a peculiar dread, recognizing the hospital’s number instantly and developing an almost Pavlovian response to let it go to voicemail.
This constant uncertainty creates a low-grade hum of anxiety that follows nurses home. There’s never a true day off when you know you might be called in, never a family gathering that can’t be interrupted by staffing emergencies. The system’s inability to maintain adequate staffing levels means nurses are perpetually on call, even during their supposed time off.
Vacation planning becomes a complex negotiation requiring months of advance notice, and even then, there’s no guarantee. I’ve seen nurses cancel long-awaited trips because the hospital couldn’t find coverage. The message is clear: your personal life matters less than the institution’s staffing needs. This structural reality never appears in nursing school brochures or orientation materials, yet it shapes our daily existence more profoundly than any clinical skill we learn.
The scheduling system itself often feels designed to maximize institutional convenience at the expense of nurse well-being. Rotating shifts disrupt sleep patterns and family routines. Last-minute schedule changes treat nurses as interchangeable parts rather than human beings with lives outside the hospital. Mandatory overtime becomes a regular occurrence rather than an emergency measure.
What makes this particularly damaging is how it interacts with the already demanding nature of nursing work. After spending twelve hours dealing with life-and-death situations, emotional trauma, and physical exhaustion, the last thing any nurse needs is to be told they must work extra hours or come in on their day off. Yet this happens routinely across healthcare facilities nationwide.
The financial pressures on hospitals often translate directly into staffing decisions that prioritize budgets over patient safety and nurse well-being. Administration may implement hiring freezes while simultaneously increasing patient loads. They might rely heavily on temporary staff or floating nurses between units where they lack specific expertise. These decisions made in boardrooms have concrete consequences on the floor—nurses stretched too thin, patients receiving less attention, errors becoming more likely.
Nurses develop complex strategies to navigate this system. We learn which managers are more flexible, which departments have better staffing ratios, which shifts are most likely to be overworked. Some nurses deliberately work night shifts or weekends because the staffing tends to be more stable, even if it means sacrificing normal social rhythms. Others, like myself, learn to move between departments when burnout looms, finding new challenges before the old ones completely consume us.
This constant adaptation comes at a cost. The energy spent navigating the system’s inefficiencies is energy not available for patient care or personal recovery. The stress of uncertain scheduling compounds the stress of clinical work. The message that our personal time is less valuable than hospital staffing needs erodes our sense of self-worth over time.
Yet within this broken system, nurses continue to show up. We develop quiet solidarity, covering for each other when possible, sharing information about which units are struggling, creating informal networks of support. We learn to advocate not just for our patients but for ourselves and our colleagues, pushing back against the most unreasonable demands while recognizing the practical limits of what we can change.
The structural challenges of healthcare staffing won’t be solved by individual nurses working harder or sacrificing more. They require systemic solutions—adequate funding, better workforce planning, realistic patient-to-nurse ratios, and genuine respect for nurses’ time and personal lives. Until then, we’ll continue developing our survival strategies, supporting each other through the chaos, and occasionally darkly joking about needing to be cold and dead before we can truly rest.
The Hidden Costs at Home
Nursing requires a particular kind of emotional accounting that extends far beyond the hospital walls. The ledger of missed moments accumulates quietly at first—a soccer game here, a parent-teacher conference there—until one day you realize the balance has shifted irreversibly. I remember standing at the nurses’ station one Saturday morning, watching through the window as parents gathered on the field across the street for what should have been my daughter’s first championship game. The pang of absence feels different when it’s measured in childhood milestones rather than shift differentials.
Children of nurses develop an understanding of sacrifice that most adults never grasp. My daughters learned early that when Mom crossed the threshold of the trauma center, she became temporarily unavailable. Not unloving, not uncaring—but committed to other people’s emergencies in ways that meant sometimes missing our own family’s important moments. They understood that the pager might go off during birthday dinners, that Christmas mornings might be cut short by call shifts, and that school performances sometimes happened without me in the audience.
This professional reality creates a peculiar form of childhood wisdom. My youngest once explained to her friend why I couldn’t chaperone their field trip: “My mom’s job is to take care of people who are having the worst day of their life. Sometimes that means she can’t be with me on my best days.” The clarity of that statement still catches in my throat years later. Children shouldn’t have to comprehend emergency priorities, but nurse’s children often do.
Guilt becomes the silent companion of every nursing professional. We learn to compartmentalize it alongside the other emotions we’re not supposed to show at work—the fear, the frustration, the grief. But guilt has a way of leaking through the partitions we carefully construct. It surfaces at 2 AM when you’re checking charts and wondering if your child remembered to practice piano. It whispers during lunch breaks when you see families visiting patients and think about your own family eating without you.
The nursing profession rarely acknowledges this particular emotional tax. We discuss burnout in terms of workplace stress and patient loads, but seldom address the domestic toll—the birthday candles blown out without us, the science projects completed with only one parent’s help, the quiet understanding that develops in children who know their parent’s work matters in ways that transcend ordinary employment.
This understanding comes at a cost. Children learn resilience but also absorb the message that other people’s crises sometimes outweigh their own needs. They become adept at reading emotional weather patterns, knowing when a particularly difficult shift has left their nurse parent too drained for bedtime stories. They develop protective instincts, often trying to shield us from additional stress at home precisely when we should be providing them comfort.
I’ve watched my colleagues navigate this delicate balance for decades. The pediatric nurse who misses her own child’s wellness checkup to care for someone else’s sick baby. The oncology nurse who stays late to comfort a dying patient’s family while her own family eats dinner without her. The ER nurse who works through the night during a mass casualty event while her child has a nightmare she can’t comfort.
These aren’t exceptional stories—they’re the daily reality of nursing. The profession demands not just our skills and knowledge, but chunks of our personal lives that we can never reclaim. No time-and-a-half pay can compensate for missing your daughter’s first steps or your son’s graduation. No amount of professional satisfaction can fully erase the memory of your child’s disappointed face when you have to leave yet another family event.
What makes this burden particularly complex is that most nurses choose this knowing the sacrifices involved. We understand the emergency nature of healthcare, the unpredictability of human bodies, the reality that sickness doesn’t respect personal schedules. Yet understanding doesn’t always prevent the quiet accumulation of regret that comes with repeated absence from family life.
The guilt manifests in subtle ways—overcompensating on days off, bringing extravagant gifts after particularly long stretches of missed events, trying to cram a week’s worth of parenting into a single day between shifts. We become experts at quality time because quantity time simply isn’t available. We learn to make moments count because we have fewer of them to offer.
This constant negotiation between professional duty and personal responsibility creates a particular kind of emotional weariness that isn’t captured in burnout surveys. It’s the exhaustion of always being pulled in two directions, of knowing that excelling at your job means sometimes failing at home, and that being present for your family might mean letting down your team at work.
Nursing schools should include courses on this reality—not to discourage prospective nurses, but to prepare them for the actual emotional mathematics of the profession. They should teach strategies for managing guilt, for communicating with family about professional demands, for creating meaningful connections despite limited time. They should acknowledge that being a good nurse often means being an absent parent, partner, or friend, and that this absence requires conscious mitigation.
The healthcare system compounds this problem by its relentless demands on nurses’ time and emotional energy. When hospitals are chronically understaffed, when overtime becomes mandatory rather than optional, when call shifts pile up during holidays—the system essentially forces nurses to choose between their professional integrity and their family commitments. This isn’t a choice any healthcare professional should have to make regularly.
I’ve seen too many excellent nurses leave the profession not because they couldn’t handle the medical challenges, but because they couldn’t reconcile the personal costs. They reached a point where missing one more birthday, one more anniversary, one more school play became emotionally untenable. The profession lost their skills not because they lacked commitment, but because the human cost of that commitment became too high.
There’s a particular irony in caring for other people’s families while your own family learns to function without you. We become experts at comforting strangers while our own children learn to self-soothe. We develop deep therapeutic relationships with patients while our personal relationships sometimes suffer from neglect. We champion other people’s well-being while occasionally compromising our own family’s emotional needs.
This isn’t a condemnation of the nursing profession—it’s an acknowledgment of its true cost. The work matters profoundly. The care we provide changes lives and sometimes saves them. But we need to be honest about what that care requires from us beyond our technical skills and medical knowledge. We need to acknowledge that nursing doesn’t just demand our time and expertise—it asks for pieces of our personal lives that we can never get back.
Perhaps the most honest thing we can tell prospective nurses is this: you will miss important moments. You will feel guilty. Your family will learn to adapt to your absence. And despite all this, you might still find the work worth doing—but go in with your eyes open about the actual price tag attached to this calling.
The Physical and Mental Toll
The emotional suppression required in nursing isn’t just psychologically draining—it manifests physically in ways we never anticipated. I remember developing tension headaches that would start around hour ten of a twelve-hour shift, a dull throbbing behind my eyes that became as regular as the medication schedule. My lower back ached from more than just lifting patients; it carried the weight of unexpressed frustrations and concerns. The stomach issues that plagued so many of my colleagues weren’t merely from irregular eating schedules but from digesting emotions we weren’t allowed to express.
Research confirms what our bodies have been telling us for decades. Chronic suppression of emotional responses leads to increased cortisol levels, which in turn contributes to hypertension, weakened immune function, and gastrointestinal problems. The very act of maintaining that professional composure—that “brave face” we were taught to wear—comes at a measurable physiological cost. We’d joke about the “nurse’s immune system” that seemed to withstand every pathogen, but the truth was more complicated. Our bodies were fighting battles on multiple fronts, and the stress of emotional labor was often the silent enemy within.
The culture of presenteeism—showing up to work regardless of personal condition—wasn’t just encouraged; it was expected. I recall working with a fever of 101 degrees because we were short-staffed, convincing myself that my patients needed me more than I needed rest. The unspoken rule was clear: unless you were hospitalized yourself, you found a way to work. This mentality extended beyond physical illness to mental health days, which were practically unheard of in most units I worked in.
Mental health support within healthcare systems remains startlingly inadequate even today. During my career, seeking counseling or therapy was often viewed as a sign of weakness rather than a professional necessity. The stigma was palpable—nurses who admitted to struggling with anxiety or depression risked being seen as unfit for duty rather than human beings responding appropriately to extreme circumstances. We were caregivers who couldn’t seek care, healers who weren’t allowed to acknowledge our own wounds.
The cumulative effect of these physical and mental health challenges creates a paradox: those trained to recognize symptoms in others become remarkably skilled at ignoring them in themselves. I can’t count how many times I advised patients about stress management while ignoring my own elevated blood pressure. We became experts at compartmentalization, but the walls between those compartments grew increasingly fragile over time.
What makes this particularly damaging is how it intersects with the natural aging process. The physical demands of nursing—long hours on our feet, lifting and turning patients, the constant motion—take their toll on the body. When combined with the physiological effects of chronic stress, the result is often premature burnout or career-ending injuries. Many excellent nurses leave the bedside not because they’ve lost their passion for patient care, but because their bodies can no longer sustain the physical punishment.
The mental health impact extends beyond our professional lives into our personal relationships. The emotional numbing that helps us survive difficult shifts doesn’t automatically switch off when we clock out. I found myself sometimes struggling to connect with family members because I’d spent twelve hours carefully moderating my emotional responses. The very skills that made me effective at my job sometimes made me distant at home, creating a different kind of toll on my personal life.
Perhaps most concerning is how this culture affects new nurses entering the profession. They witness veterans working through pain and emotional distress and internalize this as the standard to aspire to. The cycle continues not through malice but through misguided tradition, each generation passing along unhealthy coping mechanisms to the next.
Addressing these physical and mental health challenges requires more than individual resilience—it demands systemic change. Adequate staffing patterns that allow for breaks and recuperation, mental health resources that are accessible and destigmatized, and leadership that models healthy boundaries rather than praising martyrdom. Until we confront these issues honestly, we’ll continue to lose talented nurses to preventable physical and mental health crises.
The truth is, caring for ourselves isn’t a luxury or a sign of weakness—it’s a professional responsibility. Our ability to provide quality care depends on maintaining our own health, both physical and mental. Recognizing this fundamental truth might be the first step toward creating a nursing culture that sustains rather than consumes its caregivers.
The Balance Sheet of a Nursing Career
Looking back across three decades in nursing, the ledger contains entries in both black and red ink. The economic stability I sought was achieved—the student loans were paid, the mortgage stayed current, and retirement arrived with the modest comfort of a state pension. Nursing delivered exactly what I had asked of it: a recession-proof profession that provided for my family. Yet the cost columns hold entries less easily quantified but far more weighty.
The financial security came at the price of presence. I traded Christmas mornings for holiday shifts, parent-teacher conferences for night duty, and weekend soccer games for overtime that helped pay for the very cleats my children wore. These aren’t just missed events; they’re lost connections, moments that form the fabric of family life. The nursing profession doesn’t merely borrow your time—it claims pieces of your relationships, often without either party fully realizing the withdrawal until years later.
My daughter understands this calculus better than most. She watched her mother become someone else when those scrubs went on, witnessed the transformation from parent to professional that happened at the hospital threshold. Children of nurses develop a peculiar wisdom—they know that sick people need their parent more than they do, and they learn this not through lectures but through accumulated absences. They become little realists in a world that wants them to believe in superhero parents who can be everywhere at once.
Now, watching my daughter parent her own magical creatures, I see what I missed reflected in what she gives. She’s present in ways I couldn’t be, available in the moments I was always halfway out the door mentally preparing for the next shift. There’s a generosity to her parenting that comes from never having to compete with the hospital for her mother’s attention. And while I’m grateful she provides what I couldn’t, the observation comes with the sharp edge of regret.
This regret isn’t the useless kind that paralyzes—it’s the productive variety that motivates change. These days, I practice availability as a deliberate discipline. When my daughter calls, the phone gets answered. When the magical creatures want to play, the game happens immediately, not after charting fictional patients in my head. There are no more thresholds across which I become unavailable, no more shifts during which family takes second place. This is my atonement, my making-right of what nursing made wrong in our relationship dynamic.
The remarkable thing isn’t my efforts at reparation but their reception. My children have extended grace I’m not sure I would have managed in their position. They’ve forgiven the absent mother, understood the woman doing her best in an impossible system, and embraced the grandmother who finally has time. This forgiveness feels like unearned generosity, a gift given despite my having provided the conditions that made it necessary.
My relationship with nursing itself mirrors this complexity—a mixture of gratitude and resentment that defies simple categorization. The career gave me financial independence and professional competence but took emotional availability and family connection. It provided purpose but demanded personality sacrifice. It taught me about human resilience while systematically eroding my own. These aren’t contradictions but complementary truths that exist simultaneously in the heart of every long-term nurse.
This dual reality—the simultaneous thankfulness and regret—represents perhaps the most honest assessment of the nursing profession. We can acknowledge the economic stability it provides while mourning the personal costs. We can appreciate the skills gained while regretting the relationships altered. We can be proud of the care given while wishing we’d had more care to give at home. The profession doesn’t require us to choose between these perspectives—it asks that we hold them both, the gratitude and the grief, without letting either cancel out the other.
The reconciliation happens not in choosing between these competing truths but in embracing their coexistence. I can simultaneously appreciate nursing for providing for my family and wish it had taken less from our family life. I can value the financial security while mourning the emotional withdrawals. I can respect the profession while recognizing its flaws. This isn’t cognitive dissonance but mature understanding—the recognition that most things worth doing come with both benefits and costs, and wisdom lies in acknowledging both without dilution.
What remains after this accounting isn’t bitterness but clarity. The nursing profession gave what it promised economically but took more than it disclosed emotionally. The balance sheet will never show pure profit, but it doesn’t show total loss either. Like any long investment, the returns compound differently across various accounts—financial security grown steadily, emotional connections sometimes diminished, personal satisfaction fluctuating with each shift.
Perhaps this complex reckoning is what allows former nurses to finally say ‘namaste’ to the profession—not as empty gratitude or simple condemnation, but as respectful acknowledgment of something that was both difficult and meaningful, costly and valuable, damaging and formative. The word fits not because nursing was spiritually uplifting in the way the public imagines, but because the struggle itself became a kind of practice—one that eventually leads to seeing clearly what was given and what was taken, and bowing to both with equal respect.
The Truth We Carry Forward
Nurses are not angels of mercy. We never were. This profession systematically weeds out those who believe they can save everyone, who think compassion means sacrificing everything at the altar of patient care. The reality is far more complex, far more human, and far more demanding than any nursing school textbook could possibly capture.
What we do isn’t about sainthood—it’s about showing up shift after shift, year after year, knowing full well that the system will break you if you let it. We become who we need to be to face human suffering, but we never stop being human ourselves. The cost of this transformation is something nobody prepares you for, something that goes far beyond the physical exhaustion and emotional drain.
This truth needs to be spoken aloud, needs to be shared with every new student considering this path, with every administrator making staffing decisions, with every policymaker shaping healthcare regulations. The romanticized version of nursing does more harm than good—it sets impossible standards, then penalizes those who inevitably fall short. We need transparency about what this career actually demands, what it actually takes from you, and what you might never get back.
Yet within this harsh reality exists something remarkable: the resilience of ordinary people doing extraordinary work. Not because they’re angels, but because they’ve learned how to care without collapsing, how to give without disappearing, how to maintain their humanity in the face of endless need.
Looking back on three decades in scrubs, I see the pattern clearly now. The system survives because individual nurses find ways to survive within it. We develop our own methods, our own boundaries, our own small rebellions against the expectation of endless sacrifice. We learn when to say no, when to switch departments, when to protect our days off like the precious resources they are.
This hard-won wisdom deserves to be passed along, not as complaint but as necessary truth. The next generation deserves to know what they’re signing up for—the missed soccer games and Christmas mornings, the emotional toll of constant caregiving, the physical demands of long hours on your feet. They deserve to understand that setting boundaries isn’t selfishness—it’s survival.
They also deserve to know the rewards: the profound connections forged in vulnerability, the satisfaction of competent care, the financial stability that comes with a recession-proof career. It’s not all sacrifice—there’s deep meaning here, for those who approach it with clear eyes and realistic expectations.
My daughter now gives her children what I couldn’t always give her—full presence, uninterrupted attention, the luxury of a mother who isn’t constantly torn between home and hospital. In watching her, I’ve come to understand both what I missed and why I made those choices. There’s regret, yes, but also gratitude for the economic stability that allowed me to provide for my family, even when I couldn’t always be physically present.
This is the complicated truth of nursing—a career of both profound sacrifice and substantial reward, of personal cost and professional fulfillment. It doesn’t need to be romanticized to be respected. The work itself commands respect, as do the people who do it day after day, year after year, with their eyes wide open to both the beauty and the brokenness of the system.
So I’m telling you what nobody told me: this work will change you. It will demand things you didn’t know you had to give. It will show you humanity at its most vulnerable and its most resilient. And through it all, you’ll need to remember that you’re human too—not an angel, not a saint, just a person doing difficult work as well as you can for as long as you can.
Namaste.