The fluorescent lights of the urgent care clinic hummed overhead as I pressed my fingers to my throbbing temples. That’s when the nurse’s voice cut through the haze: “172 over 100 – these numbers put you at serious stroke risk.” The cardiac monitor beeped relentlessly beside me, its glowing display confirming what my pounding headache had suggested. This wasn’t supposed to happen. Not to me.
Three weeks earlier, my annual physical had shown textbook-perfect vitals – 110/70 blood pressure, resting heart rate of 58. As someone who meal-preps religiously, hits 10,000 steps daily, and swaps elevator rides for stair climbs, I’d built my identity around being ‘the healthy one’ among my friends. Now the same hands that routinely chopped kale were gripping the clinic chair as the physician explained how hypertension could silently damage organs before showing obvious symptoms.
What shocked me most wasn’t just the numbers, but the cognitive dissonance. Like many health-conscious urban professionals, I’d assumed diligent self-care created an impenetrable shield against medical crises. Yet here I was, a 42-year-old non-smoker staring down a potential cardiovascular event, realizing too late that blood pressure fluctuations often give no warning before reaching dangerous thresholds.
The nurse’s words hung in the air between beeps of the monitor: “Hypertension doesn’t care about your salad habits when it decides to strike.” In that moment, I began understanding what countless patients before me had learned – that the space between “normal” and “danger zone” can collapse without ceremony, and that even the most routine health metrics demand vigilant tracking rather than complacent trust.
As the physician reviewed my new medication instructions (amlodipine, possibly for life), my mind raced through questions so many face during unexpected diagnoses: How had multiple healthcare providers missed this progression? Why did my supposedly healthier lifestyle changes coincide with this crisis? And most urgently – what early signs had I dismissed because they didn’t fit my self-image as a wellness exemplar?
This opening scene establishes several critical themes we’ll explore:
- The silent progression of hypertension even in health-conscious individuals
- The psychological impact of sudden chronic illness diagnosis
- The limitations of relying solely on medical professionals for early detection
- The complex relationship between lifestyle changes and physiological responses
For now, know this: My journey from 110/70 to stroke-risk territory contains lessons for anyone who assumes regular exercise and clean eating guarantee immunity from health surprises. What follows is both a cautionary tale and a practical guide for navigating the gray areas where modern medicine, self-care practices, and bodily unpredictability intersect.
The Red Alert: Overlooked Hypertension Crisis
The blood pressure monitor beeped relentlessly as I sat clutching my throbbing head in urgent care. 172/100 – those flashing red numbers mocked my lifelong belief in being the picture of health. Just three weeks prior, my annual physical showed a pristine 110/70, the kind of reading that made nurses nod approvingly. Now, the urgent care physician kept glancing between my chart and the monitor with that carefully controlled neutral expression doctors master in med school.
When Numbers Tell a Different Story
My health metrics had always been my pride:
- Fitness routine: Daily 10,000 steps without fail
- Diet: Meal-prepped salads with quinoa and salmon
- Vitals: Historically textbook-perfect blood pressure
Yet the clinical reality before me painted a different picture – what the American Heart Association classifies as a Stage 2 Hypertension Crisis, dangerously close to the 180/120 threshold requiring emergency intervention. The nurse’s warning about stroke risk landed like a physical blow, leaving me mentally scrambling through recent weeks for explanations.
The Silent Progression
Looking back, the signs were there in gradual increments:
| Timeline | Blood Pressure | Clinical Response | Missed Opportunity |
|---|---|---|---|
| Baseline | 110/70 | “Ideal” | – |
| 3 months ago | 140/90 | “Probably stress” | Early intervention |
| 1 month ago | 158/90 | “White coat syndrome” | Lifestyle review |
| Present | 172/100 | Stroke risk warning | Emergency care |
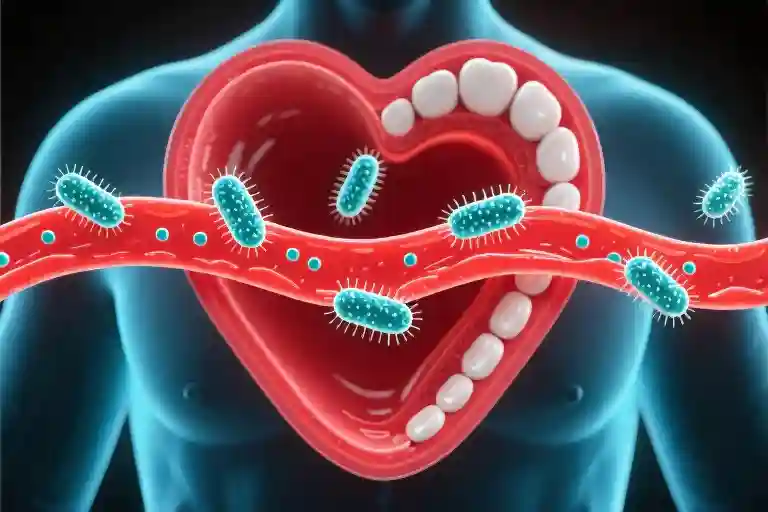
This creeping escalation embodies what cardiologists call “the hypertension paradox” – the condition often advances silently until reaching dangerous thresholds. Unlike dramatic health crises with clear symptoms, high blood pressure works like invisible termites, weakening cardiovascular structures without obvious warning signs.
Understanding the Danger Zone
That 172/100 reading placed me in territory where:
- Organ damage can occur within hours
- Stroke risk increases 4-fold compared to Stage 1 hypertension
- Medical guidelines mandate immediate evaluation
Yet the most unsettling realization? I’d walked into urgent care fully mobile, slightly headachey, but otherwise functional. Hypertension’s insidious nature means the first obvious symptom could be a catastrophic event – which explains why the CDC estimates 1 in 3 hypertensive adults don’t know they have it.
The Cognitive Dissonance of Crisis
What struck me hardest wasn’t the diagnosis itself, but the jarring disconnect between:
- My self-perception as a health-conscious individual
- The clinical reality of being minutes from a potential stroke
This mirrors findings from Johns Hopkins research on “healthy-identity bias”, where patients with strong wellness identities often delay seeking care for abnormal results. We subconsciously think “People like me don’t get seriously ill” – until the monitor proves otherwise.
Key Takeaways (So Far)
- Hypertension doesn’t care about your self-image – it progresses on its own timeline
- Small increases matter – A 30-point systolic jump warrants investigation
- Absence of symptoms ≠ absence of risk – This makes BP the ultimate silent predator
As the urgent care physician prepared my discharge papers with a new prescription, I realized this wasn’t just about starting medication. It was about fundamentally rethinking how I monitor and interpret my body’s signals – a lesson that would soon lead me down an unexpected investigative path.
Three Missed Alarms: How the Healthcare System Overlooked My Hypertension Warnings
The Pattern of Dismissal
My journey from 110/70 to stroke-risk blood pressure wasn’t an overnight catastrophe—it was a series of missed opportunities documented in three distinct medical encounters. What fascinates me most in retrospect isn’t the numbers themselves, but how differently healthcare professionals interpreted identical warning signs.
| Visit Context | BP Reading | Provider Response | Missed Risk |
|---|---|---|---|
| Rash Consultation | 140/90 | “Probably work stress” | Stage 1 Hypertension |
| Follow-up Physical | 158/90 | “Classic white coat syndrome” | Hypertensive Urgency |
| Specialist Visit | 172/100 | No emergency intervention | Stroke/Organ Damage Risk |
White Coat Syndrome: Valid Explanation or Diagnostic Crutch?
The term “white coat hypertension” describes a real phenomenon where 15-30% of patients show elevated readings in clinical settings (Mayo Clinic, 2022). But when my home readings consistently matched clinic numbers, this explanation became a dangerous dismissal. Healthcare providers often use this diagnosis as a default response to borderline high blood pressure without proper ambulatory monitoring—a practice the Journal of General Internal Medicine calls “diagnostic momentum bias.”
The Psychology of Missed Diagnoses
Three cognitive biases converged to delay my treatment:
- Anchoring Effect: The initial “stress” diagnosis became a mental shortcut
- Normalization of Deviance: Gradual BP increases seemed unremarkable
- Diagnostic Overshadowing: Focus on my rash and specialist condition diverted attention
A Johns Hopkins study found primary care providers miss approximately 56% of hypertension cases during routine visits—not from negligence, but systemic workflow issues that prioritize acute over chronic concerns.
Critical Questions I Wish I’d Asked
- “At what point would these readings concern you?”
- “What’s the protocol for verifying white coat syndrome?”
- “Can we compare today’s reading to my last three visits?”
The Turning Point
The 172/100 reading finally broke through the diagnostic inertia—not because the number itself shocked my specialist (it didn’t), but because I arrived armed with two weeks of home logs showing the same pattern. This underscores a vital lesson: Patients must become active participants in diagnostic conversations.
Pro Tip: When providers mention white coat syndrome, request ambulatory monitoring or provide 7 days of home readings before accepting this explanation.
What This Means for You
- Track Serial Measurements: Isolated readings have limited value
- Understand BP Classifications: Know Stage 1 (≥130/80) vs. Stage 2 (≥140/90) thresholds
- Recognize System Limitations: Even excellent providers work within constrained systems
My experience reveals how easily hypertension warnings can slip through healthcare’s cracks—not through malice, but through predictable cognitive patterns and system design. The solution lies in prepared patients bringing organized data to informed conversations.
{
“Article Chapter Content”: “## The Herbal Tea Paradox: When Healthy Swaps Backfire
That moment in urgent care forced me to become a health detective. As I stared at the amber liquid in my favorite mug—the same \”healthy\” herbal tea I’d been drinking religiously for months—a chilling realization hit me: my well-intentioned habit might be sabotaging my blood pressure.
The Licorice Root Connection
Most herbal tea drinkers don’t realize their favorite blends often contain licorice root, a common ingredient that packs a surprising punch. Glycyrrhizin, the active compound in licorice, mimics aldosterone, a hormone that regulates sodium retention. Here’s what my research uncovered:
- Sodium Imbalance: Glycyrrhizin can cause potassium excretion and sodium retention, forcing the heart to work harder
- Vascular Impact: Studies show licorice consumption may increase systolic BP by 3-14 mmHg within weeks ([NIH study PMC7355965])
- Cumulative Effect: Regular consumption creates a \’silent load\’ on the cardiovascular system
My \’healthy\’ three-cups-a-day habit had unknowingly become physiological Russian roulette.
The Experiment That Changed Everything
Armed with this knowledge, I conducted a simple self-experiment:
| Day | Herbal Tea Intake | Morning BP | Evening BP | Notes |
|---|---|---|---|---|
| 1-3 | 3 cups daily | 152/92 | 164/98 | Baseline measurement |
| 4-6 | 1 cup daily | 146/88 | 158/94 | Slight improvement |
| 7-9 | Zero intake | 138/84 | 142/86 | Significant drop |
| 10+ | Reintroduced | 148/90 | 156/96 | Immediate rebound |
The results were undeniable. While not scientifically rigorous, this personal data mirrored clinical findings about licorice’s hypertensive effects.
Beyond the Tea Cup: A Framework for Healthy Swaps
This experience taught me to evaluate lifestyle changes through a risk-aware lens:
1. The Replacement Audit
- What exactly am I substituting? (In my case: soda → herbal tea)
- Have I researched all active ingredients?
- Does this align with my specific health conditions?
2. The Transition Timeline
- Document changes alongside health metrics
- Note any new symptoms within 2-8 weeks
- Compare pre/post biomarkers if possible
3. The Professional Checkpoint
- \”I\’ve switched from X to Y—should we monitor anything?\”
- Ask about nutrient interactions (e.g., licorice + potassium levels)
- Request baseline/tracking tests if warranted
When \”Natural\” Doesn\’t Mean Neutral
Common \’healthy\’ alternatives that warrant caution:
- Energy Bars → May contain hidden sodium (some have 300mg+ per serving)
- Kombucha → Fermentation creates histamines that can affect some individuals
- Plant Milks → Certain thickeners may impact medication absorption
- Essential Oils → Some (like rosemary) can elevate BP when used aromatically
The Mindful Transition Protocol
Now, any lifestyle change follows my 5-step system:
- Research Phase: 48 hours investigating potential downsides
- Trial Period: 2-week limited introduction with tracking
- Biomarker Check: Compare key health metrics pre/post
- Professional Consult: Quick telehealth check-in if needed
- Long-Term Monitoring: Ongoing observation for delayed effects
Your Turn: Becoming an Informed Health Advocate
As I learned the hard way, even positive changes require due diligence. That \’healthy\’ herbal tea I loved? Turns out it contained three BP-raising herbs I\’d never thought to investigate. Now my morning ritual includes reading ingredient labels as carefully as nutrition facts.
Pro Tip: Download our Herbal Ingredient Safety Cheat Sheet to quickly check common interactions.
Next time you make a \’healthy\’ swap, ask yourself: Do I truly understand what\’s in this cup (or package or bottle)? Your cardiovascular system will thank you for that extra moment of consideration.”
}
4. Survival Toolkit: Becoming a Smart Blood Pressure Manager
That urgent care visit was my wake-up call. When the doctor casually mentioned I might need medication for life, it hit me – I needed to take control. Here’s what I’ve learned about managing blood pressure like a pro.
The Golden Four Rules of Home Monitoring
1. Timing is Everything
- Morning routine: Measure within 1 hour of waking (before coffee)
- Evening check: Before dinner or bedtime medications
- Bonus reading: Once midday when possible
Pro tip: Keep a log – I use a simple spreadsheet with timestamps and notes about activities beforehand.
2. Posture Perfection
After getting inconsistent readings, my cardiologist demonstrated the right way:
- Sit quietly for 5 minutes first (no checking BP right after climbing stairs!)
- Back supported, feet flat, arm at heart level
- Cuff directly on skin – no bulky sweaters underneath
3. Device Matters
Not all home monitors are created equal. Look for:
✔ FDA-cleared validation (check www.validatebp.org)
✔ Upper arm cuffs (wrist monitors often less accurate)
✔ Memory function to track trends
My pick: Omron Platinum – it syncs with health apps automatically.
4. Record Like a Scientist
I created a system that finally made sense to my doctor:
📊 Weekly averages (discard the highest/lowest each week)
📝 Symptom journal (headaches? dizziness? log it)
🎯 Target zones color-coded (green/yellow/red based on my personal thresholds)
Talking to Your Doctor: 3 Essential Questions
After being dismissed multiple times, I prepared these conversation starters:
- “At what specific reading would you recommend medication?”
Why it works: Moves beyond vague “high BP” discussions to concrete action thresholds. - “Could we rule out secondary causes before assuming it’s essential hypertension?”
My experience: This prompted tests that found mild kidney artery narrowing. - “How should I adjust monitoring if I’m trying lifestyle changes?”
Key insight: My doctor suggested checking before/after new supplements or diet changes.
Calcium Channel Blockers: What I Wish I Knew
When prescribed amlodipine, I researched proper usage:
🕒 Timing: Take at same time daily (I set a 7pm phone reminder)
🍊 Interactions: Grapefruit is a no-go – it boosts medication potency dangerously
📈 Monitoring: Expect gradual effect (full benefits take 1-2 weeks)
⚠️ Side effects: Swollen ankles are common but report dizziness immediately
Visual guide: [Insert simple infographic showing amlodipine dos/don’ts]
Building Your Personal Early Warning System
Combining professional advice with personal observation created my safety net:
🔔 Alert threshold: If home readings exceed 150/95 for 3 consecutive days → call doctor
🔍 Investigation mode: Any sudden spike triggers a habit audit (new foods? stress? sleep changes?)
🤝 Accountability partner: My spouse knows to ask “Did you check today?” without nagging
Remember: These numbers aren’t just data points – they’re vital conversations between you and your body. My “healthy” herbal tea mistake taught me that even well-intentioned changes need monitoring. Now when I see those home readings in the safe zone, it’s not just relief – it’s empowerment.
Redefining Health: Finding Certainty in Uncertainty
That moment in urgent care became my wake-up call. As I sat clutching my headache with those terrifying numbers flashing on the monitor—172/100—I realized everything I thought I knew about health needed reevaluation. This final chapter isn’t just about blood pressure management; it’s about developing a new lens for viewing wellness in our complex biological systems.
The Five Dimensions of Personalized Health Monitoring
- Biometric Literacy
Understanding numbers beyond ‘normal ranges’:
- My 110/70 baseline mattered more than textbook ‘120/80’ standards
- Tracking diurnal patterns (morning surges vs. evening dips) proved crucial
- Intervention Impact Mapping
Creating your personal cause-effect ledger: Change Introduced Timeframe Biometric Impact Herbal tea (3 cups/day) Week 2-4 +22mmHg systolic Amlodipine 2.5mg Day 5-7 -15mmHg systolic - Environmental Forensics
Decoding hidden influencers:
- That ‘stressful’ work meeting correlated with +8mmHg spikes
- Hydration levels affected readings more than caffeine ever did
- Healthcare Team Dynamics
Building your diagnostic dream team:
- Primary care physician for baseline management
- Cardiologist for medication fine-tuning
- Nutritionist specializing in herb-drug interactions
- Psychological Readiness
Preparing for the emotional labor of chronic care:
- The grief cycle of accepting lifelong medication
- Reframing ‘patient’ to ‘health CEO’ mentality
The Unexpected Effects Checklist
Before making any health change—whether it’s trendy superfoods or new workout routines—run through this safety audit:
- Biochemical Cross-Checks
- Could this interact with medications? (Even ‘natural’ supplements like St. John’s Wort)
- Does it affect absorption of nutrients? (Like grapefruit with statins)
- Adaptation Period
- Allow 2-4 weeks for baseline stabilization after changes
- Watch for rebound effects (my BP initially dropped too low on meds)
- Data Triangulation
- Correlate with sleep trackers, stress journals, menstrual cycles
- My Apple Watch revealed nocturnal BP patterns my doctor missed
- Cultural Assumptions
- Question ‘healthy’ labels (my ‘detox’ tea contained hypertension-triggering licorice root)
- Recognize socioeconomic factors (fresh produce access affects dietary changes)
Full Circle: The ER Revisited
That panicked version of me in urgent care—clutching the gurney rails while nurses scrambled—could never have imagined the silver lining. Today, I carry not just a pillbox, but something far more powerful: the ability to participate in my care with informed curiosity rather than fearful compliance.
When my new primary care physician recently noted my 118/76 reading, she asked what I’d changed. This time, I could walk her through not just the numbers, but the story behind them—the failed experiments, the accidental discoveries, the hard-won wisdom that transformed me from a passive patient to an active health detective.
Because true wellness isn’t about avoiding all risks or finding perfect solutions. It’s about developing the discernment to navigate uncertainty, the humility to question our assumptions, and the courage to keep rewriting our health narratives—one measured, mindful choice at a time.
Your Turn: Download our Health Intervention Impact Tracker to start mapping your personal biometric story. Because the most powerful health insights often hide in the spaces between ‘normal’ and ‘not quite right.’
Rethinking Health: Finding Certainty in Uncertainty
That moment in urgent care changed everything. The flashing 172/100 on the monitor didn’t just represent numbers—it shattered my assumptions about what being “healthy” truly means. If there’s one lesson this hypertension crisis taught me, it’s this: wellness isn’t about perfect choices, but about becoming an active investigator of your own body.
The Paradox of Healthy Living
We’ve all seen the inspirational stories—someone switches from soda to green tea, starts yoga, and transforms their health. But my experience revealed the uncomfortable truth: even well-intentioned changes can backfire. When I replaced my occasional diet soda with “healthy” herbal tea, I never imagined certain herbs could interfere with blood pressure regulation. This isn’t to demonize herbal remedies, but to highlight a critical gap in how we approach lifestyle changes:
- The Monitoring Gap: We track finances with apps, but often guess at health impacts
- The Individuality Gap: What works for 90% may harm the 10% with unique physiology
- The Data Gap: Single-point measurements (like annual physicals) miss trends
Your Personal Health Detective Kit
Through this journey, I developed five practical dimensions for smarter health monitoring:
- Baseline Awareness
- Know your normal ranges (not just textbook norms)
- Example: My “healthy” 110/70 made 140/90 seem catastrophic
- Change Correlation
- Maintain a simple log linking habits to metrics
- Pro tip: Note new supplements/foods alongside measurements
- Multi-Source Verification
- Compare professional readings with home monitoring
- Crucial for identifying white coat syndrome vs real issues
- Contextual Understanding
- Research how interventions might affect your conditions
- Surprising fact: Licorice root (in some herbal teas) can raise BP via glycyrrhizin
- Professional Dialogue
- Come to appointments armed with data, not just symptoms
- Try: “Doctor, I’ve recorded three weeks of home readings—can we review the trend?”
When Healthy Choices Aren’t Enough
That emergency room visit forced me to confront healthcare’s uncomfortable reality: the system often misses gradual changes until they become emergencies. The table below shows how my rising BP slipped through the cracks:
| Visit | BP Reading | Professional Response | What Was Missed |
|---|---|---|---|
| Rash Check | 140/90 | “Just stress” | 30-point jump from baseline |
| Follow-Up | 158/90 | “White coat effect” | Consistent elevation pattern |
| Specialist | 172/100 | No urgent action | Stage 2 hypertension criteria met |
This isn’t about blaming individuals—it’s about recognizing that we must become active partners in our care.
The Unexpected Effects Checklist
Now, before making any health change, I ask:
- Timing: When did I start this, and when did changes appear?
- Research: Are there documented interactions with my conditions?
- Monitoring: What metrics should I track to assess impact?
- Duration: How long until I can reasonably expect results?
- Exit Plan: If this doesn’t work, what’s my alternative?
Returning to the Beginning
As I look back at that panicked moment seeing the stroke-risk numbers, I realize the true lesson wasn’t about avoiding herbal tea or trusting doctors more—it was about developing what researchers call “critical health literacy.” The ability to:
- Question assumptions (even about “healthy” choices)
- Connect dots across time and data points
- Advocate effectively within medical systems
Final Thought: That blood pressure monitor didn’t just display numbers—it showed me how fragile our health narratives can be. But here’s the hopeful part: with the right tools and mindset, we can write better ones.
Download our free 7-Day Blood Pressure Tracker to start your own health detective work. (Includes medication logs, symptom notes, and doctor question prep sections)
Disclaimer: This narrative reflects one individual’s experience. Always consult healthcare providers before making medical decisions. Herbal interactions vary by person and preparation.