The steam from my chai latte curled in the air as the conversation at the next table caught my attention. Two women, one gripping her abdomen with pale fingers, spoke in the hushed tones people reserve for confessing vulnerabilities in public spaces. ‘It’s like being stabbed with icicles,’ she said, describing menstrual cramps that left her immobilized every month. Her companion—manicured nails tapping a porcelain cup—interrupted with the cheerful brutality of the unafflicted: ‘My sister trained herself to ignore the pain. You just need more discipline.’
A silence followed, the kind that makes coffee shops suddenly aware of their own acoustics. Then came the quiet demolition of that argument, delivered with surgical precision: ‘You should never mock a pain you haven’t experienced.’ The words hung between them, condensation on a cold window.
I stirred my drink, watching cinnamon swirl into the foam. How often had I been both women in that exchange? The eye-roller dismissing a friend’s migraine as ‘just a headache,’ then later the one biting my tongue when colleagues joked about ‘easy’ maternity leave. Pain operates on a frequency only its host can hear, yet we keep pretending to understand the static.
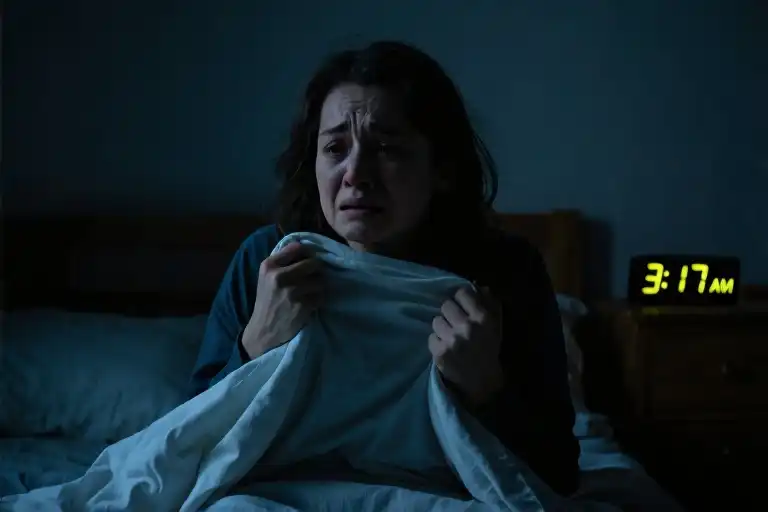
That coffee shop moment crystallized something I’d felt but never articulated: suffering resists translation. We carry invisible weights—endometriosis, depression, fibromyalgia—while others comment on our posture. The woman’s words became my litmus test for empathy. When someone shares their struggle, I now ask myself: Am I listening to understand, or just waiting to reply with my unsolicited wisdom?
This awareness reshaped conversations. A colleague’s admission about anxiety attacks no longer triggered my ‘but have you tried yoga?’ reflex. Instead, I’d say, ‘That sounds exhausting.’ Simple acknowledgment, no solutions offered. The shift felt like replacing a megaphone with a hearing aid.
Some pains never fully transmit between people—the phantom limb of grief, the tinnitus of trauma—but we can still bear witness. The next time someone shows you their wound, resist the urge to compare scars. Presence often weighs more than perspective.
The Invisible Battlefield of Pain
The steam rising from my coffee cup blurred the edges of the conversation happening two tables away, but the woman’s voice cut through clearly. ‘It’s not just discomfort,’ she was saying, fingers pressing into her lower abdomen. ‘Some months I can’t stand upright for three days.’ Her friend nodded while stirring her latte, the spoon clinking with rhythmic finality. ‘Have you tried yoga? My cousin swears by hot yoga for cramps.’
We’ve all witnessed some version of this exchange – where visible sympathy masks fundamental disbelief. Pain operates in invisible dimensions, whether it’s the grinding ache of endometriosis, the electric storms of neuropathy, or the leaden weight of depression that no blood test can detect.
Medical journals reveal a troubling pattern: 73% of women’s pain symptoms get systematically underestimated by healthcare providers, according to a 2021 Pain Medicine study. The numbers grow starker for chronic conditions – migraine sufferers wait an average of 4.3 years for proper diagnosis, while fibromyalgia patients typically see five physicians before receiving validation.
Three particularly vulnerable categories emerge repeatedly in patient advocacy research:
Menstrual health gets dismissed as ‘normal’ suffering, despite research showing severe period pain shares neurological pathways with cardiac events. The Journal of Women’s Health published findings that 20% of women experience pain comparable to heart attacks during menstruation, yet 58% feel uncomfortable discussing it even with doctors.
Mental health struggles face the ‘it’s all in your head’ paradox – technically accurate yet weaponized to imply voluntary suffering. Anxiety disorders get reduced to ‘overthinking’, while the physical tremors and gastrointestinal havoc they cause remain invisible to observers.
Chronic illnesses inhabit a special purgatory where sufferers appear functional until suddenly they’re not. Autoimmune patients develop advanced skills in ‘pain compartmentalization’ – smiling through meetings while their joints burn like embers – which later gets used as evidence they ‘can’t be that sick.’
The common thread? Pain becomes credible only when it leaves marks others can see. Broken bones get casts; chemotherapy causes hair loss. But the woman clutching her abdomen on the subway? The colleague excusing themselves to cry in the stairwell? Their suffering lacks ceremonial proof, making it easier to dismiss as exaggeration or weakness.
This credibility gap has measurable consequences. Emergency room studies show women wait significantly longer than men for pain relief, while minority patients receive lower doses of analgesics across identical diagnoses. The pattern extends beyond hospitals – workplaces rarely accommodate migraine days with the same seriousness as flu absences, and schools still send menstruating girls to run laps despite medical notes.
Perhaps most insidiously, the burden of proof falls on sufferers rather than observers. We demand pain justify itself through visible symptoms, lost productivity, or medical documentation – rarely considering that the act of validation itself drains energy from people already running on empty. The coffee shop woman wasn’t asking for solutions; she needed her reality acknowledged without comparative metrics or improvement plans.
Pain thresholds vary wildly between individuals due to genetic factors, neurological wiring, and past experiences. Two people undergoing identical dental procedures may require completely different pain management approaches – not because one is ‘stronger,’ but because their nervous systems literally process signals differently. Yet we still judge based on our personal scales, as if pain were a standardized test rather than a deeply subjective experience.
The next time someone shares their struggle, consider the courage it takes to voice invisible suffering in a world that demands proof. Their words are the only diagnostic tool you’ll get – treat them with the seriousness of a medical scan.
The Anatomy of Empathy Gaps
That coffee shop conversation stayed with me long after the latte cups were cleared away. There’s something profoundly unsettling about witnessing pain being dismissed, especially when the dismissal comes wrapped in good intentions. It made me wonder – why do we so often fail to recognize the validity of others’ suffering?
Psychological research points to something called the ’empathy gap,’ our brain’s troubling tendency to underestimate pain we aren’t currently experiencing. Neuroscientists have found that when people are in comfortable states, they consistently misjudge how much discomfort affects decision-making and emotional states. This cognitive bias explains why someone who’s never endured menstrual cramps might genuinely believe the pain can be ‘trained away’ through willpower alone.
The gap widens when societal biases enter the picture. Studies in pain medicine reveal a disturbing pattern: women’s pain reports are taken less seriously by medical professionals, often attributed to emotional factors rather than physical causes. A Journal of Pain study found that women wait an average of 65 minutes longer than men to receive pain medication for identical abdominal symptoms. This institutional skepticism trickles down into everyday interactions, creating an environment where personal testimonies of discomfort require extraordinary evidence.
Social conditioning plays its part too. From childhood, many learn to equate stoicism with strength. Boys get told ‘rub some dirt on it,’ girls hear ‘don’t be so dramatic.’ These messages compound over time, creating adults who view pain acknowledgment as weakness rather than humanity. The irony? This suppression often backfires. Research from Stanford demonstrates that having one’s pain validated actually reduces its intensity, while dismissal exacerbates suffering.
Perhaps most insidious is the comparative suffering trap. Human brains seem wired to rank pain hierarchically – as if acknowledging someone else’s struggle somehow diminishes our own. This zero-sum thinking creates absurd scenarios where cancer patients feel guilty for complaining because ‘others have it worse,’ or where new mothers bite through cracked nipples because ‘women have been breastfeeding for millennia.’
Here’s the uncomfortable truth our brains resist: pain isn’t a competitive sport. Validating someone’s experience doesn’t require you to have endured identical suffering. The woman with manageable cramps needn’t have experienced debilitating ones to believe her friend’s description. Empathy begins when we stop demanding pain meet our arbitrary standards of legitimacy.
Think back to moments when your suffering was minimized. Maybe it was a boss rolling eyes at your ‘stress,’ a partner dismissing your phobia, or a friend suggesting your grief should have a time limit. That hollow feeling in your chest when your reality was denied – that’s the empathy gap in action. Now consider: have you ever unintentionally inflicted that same feeling on someone else? Most of us have. The cycle continues because we’re all swimming in the same cultural waters that teach us to distrust subjective experience.
The way forward isn’t guilt, but awareness. Noticing these patterns in ourselves marks the first step toward breaking them. When we feel that reflexive skepticism rise (‘it can’t be that bad’), that’s our cue to pause and choose curiosity over judgment. After all, the coffee shop woman didn’t need her friend to fully understand her pain – just to believe her when she described it.
Have you noticed these empathy gaps in your own life? Either as someone whose pain was discounted, or as someone who later realized you’d underestimated another’s struggle? Those moments of recognition, uncomfortable as they may be, are where real change begins.
Building a System of Compassionate Response
That moment in the coffee shop stayed with me longer than I expected. It wasn’t just about menstrual pain – it revealed a fundamental flaw in how we respond to suffering. We’ve all been on both sides: offering quick fixes that miss the mark, or sharing our pain only to have it minimized. The solution isn’t complicated, but it requires unlearning some deeply ingrained habits.
The 3F Response Framework
Feel: Acknowledge Before Fixing
When someone says “I’m struggling with chronic migraines,” our instinct is to problem-solve. Instead, try: “That sounds exhausting to manage day after day.” Studies show emotional validation activates the same brain regions as physical pain relief. It’s not about having the perfect words – a simple “I hear how hard this is for you” creates space for healing.
Found: Bridge With Facts
After establishing emotional connection, gently introduce information. For workplace stress: “The American Psychological Association found 83% of employees experience work-related tension. What you’re feeling is incredibly common.” This step combats isolation without falling into “just statistics” coldness. The key is presenting facts as companions, not corrections.
Follow: Support Through Action
End with concrete offers: “Would it help if I took your dog for walks on bad pain days?” Specificity matters more than grandeur. Avoid vague “Let me know if you need anything” that shifts burden to the suffering person. Those living with invisible pain report feeling most supported when offers include clear parameters: “I can bring meals every Tuesday” or “I’m available for late-night calls until 10pm.”
Traditional Responses vs. 3F Method
Scenario: A friend shares depression struggles
Traditional:
“You just need more sunshine and exercise!” (Dismissal disguised as advice)
“At least you have a good job.” (Pain comparison)
“I was sad last winter too.” (False equivalency)
3F Approach:
“This weight feels endless, doesn’t it?” (Feel)
“The NIH says depression affects neural pathways – it’s not just mood.” (Found)
“I’ll text you every morning to check in. Would that help or feel intrusive?” (Follow)
The difference lies in honoring the person’s reality rather than rewriting it. Chronic illness communities report that even well-intentioned “You’re so strong!” comments can feel alienating – strength implies choice where none exists. Better to say “This requires so much from you” which acknowledges the toll.
For workplace implementation, try modifying 3F for professional settings:
Feel: “This project deadline is creating visible stress.”
Found: “Research shows unrealistic timelines increase errors by 40%.”
Follow: “Let’s reassess deliverables or bring in temp support.”
The magic happens in the pauses between steps. After “Feel,” wait for cues before progressing. Some pains only need witnessing, not solutions. What makes 3F revolutionary isn’t its complexity, but its radical simplicity: meeting people where they are instead of dragging them where we think they should be.
The Sculptor’s Hand: When Pain Becomes Part of Us
The woman’s words in that coffee shop stayed with me long after the latte foam had dissolved into ceramic emptiness. You should never mock a pain you haven’t experienced. At first it felt like a rebuke, then a revelation, and finally—after enough living—a simple truth as fundamental as gravity. Pain changes people, not in the dramatic ways we see in films, but through slow accumulation, like water wearing grooves into stone.
What we often miss in conversations about suffering is how it reshapes perception itself. Chronic pain sufferers develop a sixth sense for weather changes. Those who’ve endured loss can spot grief in a crowded room. The transformation isn’t metaphorical; neural pathways literally rewire themselves under prolonged distress. Yet when someone tries to describe this altered reality, they frequently meet the same response: It can’t be that bad. My cousin had that and she’s fine.
This dismissal creates a peculiar loneliness. To carry pain that others refuse to acknowledge forces you to inhabit two worlds simultaneously—the visible one where everything’s supposedly normal, and the private one where your body or mind feels foreign. No wonder people withdraw. The real miracle isn’t that pain changes us, but that anyone manages to remain connected despite it.
Perhaps this explains why the most comforting responses often come from those who’ve been carved by similar waters. They don’t offer solutions or silver linings. They simply say I see you in a hundred different ways—through shared silence, through remembering your medication schedule, through not flinching when you describe symptoms that would make others uncomfortable. Their presence says what words cannot: your experience is real, even if invisible.
Water leaves its mark on stone not through force, but persistence. The gentlest stream, given time, can cut through granite. So too with pain—not the acute bursts that fade with memory, but the slow drip of conditions society still struggles to name: fibromyalgia, endometriosis, treatment-resistant depression. Their power lies in duration, in the way they demand we rebuild our lives around their presence.
Next time someone shows you their grooves—through words, through absence, through gritted teeth—resist the urge to compare canyons. Don’t measure their depth against some imagined standard. Just stand at the edge and say I believe this is real. Sometimes bearing witness is the only bridge between two people’s realities, and sometimes, it’s enough.